The Developing Skin Barrier: What Parents Should Know
Jan 2, 2026
The Developing Skin Barrier: What Parents Should Know
If I told you that your baby's skin is working harder right now than it ever will in their entire life, would you believe me? It's true. In these precious early months and years, your little one's skin isn't just lying there looking adorable (though it absolutely is)—it's constructing one of the most sophisticated defense systems the human body possesses.
The skin barrier. You've probably heard the term thrown around in skincare ads and parenting articles, but what does it actually mean? And more importantly, why should you care about something you can't even see?
Let me paint you a picture that might help this click into place.
Your Baby's Invisible Construction Site
Imagine your baby's skin as a house being built from the ground up. The foundation is there, the frame is up, but the walls aren't quite finished, the insulation has gaps, and the roof is still getting its final weatherproofing. That's essentially what's happening on the microscopic level of your baby's skin every single day.
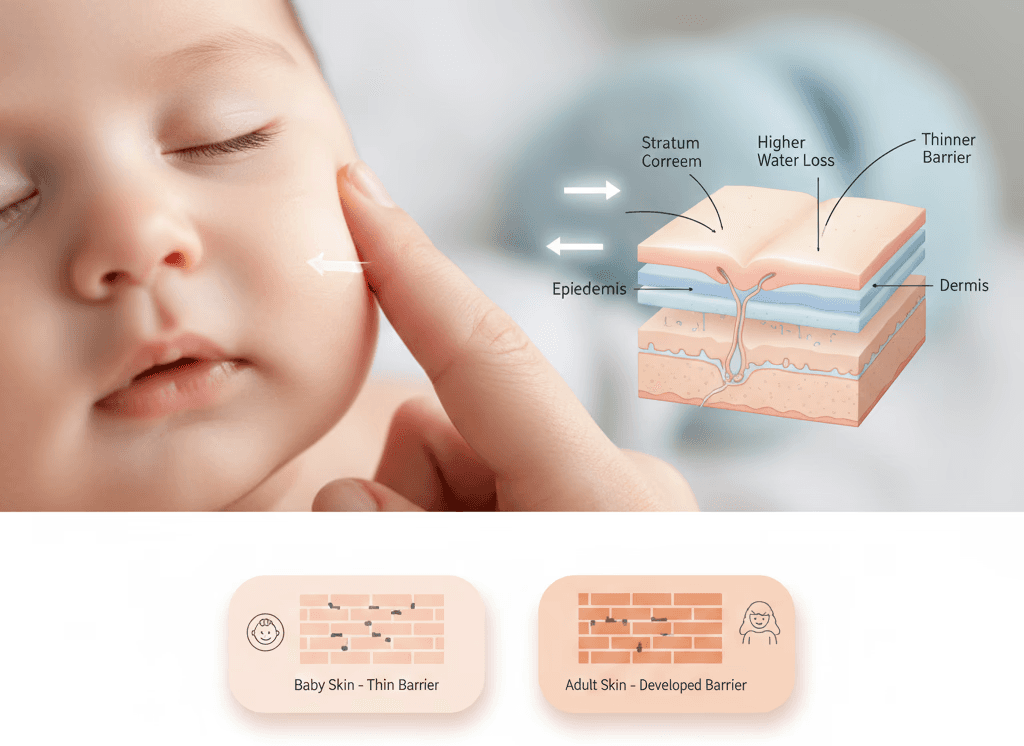
This construction project—technically called the stratum corneum, or skin barrier—is the outermost layer of skin that keeps the good stuff in (moisture, nutrients, protective oils) and the bad stuff out (bacteria, irritants, allergens, harsh environmental elements). In adults, this barrier is fully mature and remarkably efficient. In babies? It's a beautiful, complex work in progress.
According to research from the International Journal of Cosmetic Science, a baby's skin barrier doesn't reach full maturity until somewhere between 12 months and 2 years of age, though some aspects continue developing even longer (source). That means for all those months when your baby seems impossibly delicate—they genuinely are.
The Science That Will Change How You See Baby Skin
Let's get into the fascinating biology of what's actually happening. Your baby's skin is about 20-30% thinner than yours—I mentioned this in our previous discussion, but it bears repeating because the implications are huge. But thickness is just one part of the story.
Here's what else is different about your baby's developing barrier:
The lipid layer is still organizing itself: Think of this like the mortar between bricks. In adult skin, natural fats (lipids like ceramides, cholesterol, and fatty acids) form tight, organized layers that lock moisture in and keep irritants out. In baby skin, these lipids are present but not yet arranged in that protective pattern. Studies using electron microscopy show that infant skin lipids don't achieve adult-like organization until after the first year (source).
Transepidermal water loss (TEWL) is higher: This technical term simply means water evaporates from your baby's skin much faster than from yours—approximately 2.4 times faster in newborns, according to dermatological research. Picture a sponge with larger holes versus one with tightly packed pores. Your baby's skin is the former, which is why babies can dehydrate more quickly and why their skin feels dry even when you think you've applied enough moisturizer.
The corneocytes are smaller and more loosely connected: These are the actual skin cells that form the outermost layer. In babies, they're smaller and the connections between them (called corneodesmosomes) are fewer and weaker. Imagine a cobblestone path with large gaps versus tightly fitted paving stones. Substances can slip through those gaps more easily in baby skin, both in and out.
The skin's pH is higher: Newborns start with a skin pH around 6.5, which gradually becomes more acidic (lowering to around 5.5) over the first few months. This matters because the slightly acidic pH of mature skin is crucial for preventing bacterial growth and maintaining healthy skin flora. Research in the journal Pediatric Dermatology shows this pH transition is critical for establishing the skin's antimicrobial defense (source).
What This Means for Your Daily Care Routine
Understanding the biology isn't just academic—it directly impacts the choices you make every single day. Let me walk you through a typical day in your baby's life and show you where this matters.
Morning wash: When you wipe your baby's face or give them that morning clean-up, even plain water can be disruptive if overused. Water, surprisingly, is quite good at stripping away those protective lipids we talked about. This is why babies who are bathed too frequently (more than once daily) often develop dry, irritated skin. The American Academy of Pediatrics recommends bathing babies just 2-3 times per week until they're crawling and getting genuinely dirty (source).
Diaper changes: The diaper area faces a unique challenge. It's occluded (covered), exposed to moisture and waste products, and changed multiple times daily. This environment can compromise the skin barrier quickly. Research shows that diaper dermatitis (diaper rash) affects up to 50% of infants, primarily because the constant moisture and friction overwhelm the developing barrier's ability to protect itself.
Afternoon moisturizing: This isn't just about soft skin—it's about actively supporting barrier development. When you apply a proper moisturizer, you're providing those lipids and moisture-retaining ingredients that help fill in the gaps while your baby's skin is still learning to produce and organize its own.
Evening routine: By the end of the day, your baby's skin has been exposed to air, clothing friction, cleaning, products, and environmental stressors. Even indoor air—especially heated or air-conditioned environments—can challenge that developing barrier. Studies show that humidity below 40% can significantly increase TEWL in infants, essentially dehydrating their skin as they sleep.
The Critical First Three Months
Pediatric dermatologists often talk about the "fourth trimester" for skin. Just as babies are completing their development outside the womb in so many ways, their skin is making a massive adjustment.
In utero, your baby's skin was surrounded by amniotic fluid—a perfectly balanced, temperature-controlled, sterile environment. The moment they're born, everything changes. Suddenly, this skin is exposed to air, temperature fluctuations, fabrics, products, bacteria, and a completely different moisture environment.
The first twelve weeks are when the most dramatic barrier development occurs. Research tracking infant skin biophysics found that skin hydration, elasticity, and barrier function all show significant maturation curves in the first 90 days of life (source). This is your baby's skin speedrunning the construction project we talked about.
During this time, you might notice:
Peeling skin: Especially in the first two weeks, this is completely normal. It's literally the outer layer of skin that developed in utero shedding to make way for the new skin adapted to air exposure.
Dry patches: Even with moisturizing, some areas (like hands, feet, and cheeks) may seem persistently dry. This is that higher TEWL at work, combined with these areas getting more environmental exposure.
Sensitivity to temperature: Babies often develop rashes or blotchy skin in response to heat or cold because their barrier isn't yet efficient at regulating the skin's response to temperature changes.
Cradle cap: Those flaky patches on the scalp are related to sebum (oil) production and skin cell turnover as the barrier establishes itself. It typically resolves as the barrier matures.
When Things Go Wrong: Barrier Dysfunction
Sometimes, despite your best efforts, your baby's skin barrier struggles. This can manifest in several ways, and understanding them helps you respond appropriately.
Eczema (Atopic Dermatitis): This affects approximately 20% of infants in developed countries, according to the National Eczema Association (source). While genetics play a significant role, eczema is fundamentally a barrier dysfunction disorder. The skin can't retain moisture properly and allows allergens and irritants to penetrate more easily, creating a cycle of inflammation and further barrier damage.
I spoke with Amanda, a mother whose daughter developed eczema at four months. "I felt like I was doing everything right," she told me. "Gentle products, regular moisturizing. But her skin was still angry and red. When we saw a pediatric dermatologist, I learned that my daughter's skin needed more intensive barrier support than typical baby skin—prescription moisturizers with specific lipid ratios that mimicked what her skin wasn't producing properly."
Contact dermatitis: This occurs when something touches the skin and causes irritation or an allergic reaction. With a developing barrier that's more permeable, babies are more susceptible. Even products labeled as baby-safe can cause reactions if they contain problematic ingredients or if they're used too frequently, overwhelming the barrier's resilience.
Infections: When the barrier is compromised, bacteria and fungi that normally can't penetrate the skin find their way in. Staph infections, thrush, and other conditions become more likely. Research shows that infants with impaired barrier function are three times more likely to develop skin infections in their first year.
Supporting Healthy Barrier Development: The Essentials
The good news? You can actively support your baby's skin barrier development with some straightforward practices. Think of yourself as the project manager overseeing that construction site we talked about—you're providing the right materials and conditions for the work to progress smoothly.
Less is more with cleansing: This might be the single most important thing you can do. Every time you use soap or cleanser, you're removing some of those precious lipids. For newborns and young infants who aren't mobile yet, plain water is often sufficient for most cleaning. Save actual cleansers for genuinely dirty situations or the diaper area.
When you do use cleansers, choose ones specifically formulated to match baby skin's pH and that contain gentle surfactants. The term "soap-free" or "syndent" (synthetic detergent) is actually positive here—these are typically gentler than traditional soaps, which have a high pH that can disrupt the skin barrier.
Strategic moisturizing: The best time to moisturize is within three minutes of bathing or washing, while the skin is still slightly damp. This locks in the water your baby's skin has absorbed. But here's what matters most: what you're applying.
Look for moisturizers that contain:
Ceramides: These are identical to the lipids naturally found in skin and directly support barrier structure
Glycerin or hyaluronic acid: These humectants draw moisture into the skin and help it stay there
Petrolatum or dimethicone: These occlusives create a protective seal that reduces water loss
A study published in the Journal of Allergy and Clinical Immunology found that daily moisturizing from birth with barrier-supporting creams reduced the risk of developing eczema by 50% in high-risk infants (source). That's not a small number—that's profound protection achieved through something as simple as daily moisturizing.
Gentle fabrics and proper washing: Your baby's clothes and bedding are in constant contact with their skin. Choose soft, breathable fabrics like cotton. Wash new items before use to remove manufacturing chemicals and fabric finishes. Use fragrance-free, dye-free detergents and skip fabric softeners, which leave residue that can irritate sensitive skin.
Environmental humidity: Remember that TEWL we discussed? You can reduce it by maintaining proper humidity in your home, ideally 40-60%. A simple humidifier in your baby's room, especially during winter months or in air-conditioned homes, can make a measurable difference in skin hydration.
Sun protection: UV radiation damages the skin barrier directly and generates free radicals that interfere with healthy barrier development. For babies under six months, sun avoidance and protective clothing are primary. After six months, mineral-based sunscreens (zinc oxide or titanium dioxide) create a physical barrier without chemical absorption, making them ideal for developing skin.
The Microbiome Connection
Here's a fascinating dimension you might not have considered: your baby's skin isn't sterile, and that's a good thing. The skin microbiome—the community of bacteria, fungi, and other microorganisms that live on the skin surface—is an integral part of the barrier system.
In the first year of life, this microbiome is establishing itself, and it plays a crucial role in barrier development. Beneficial bacteria produce antimicrobial peptides that fight off harmful pathogens, modulate the immune system, and even influence the production of lipids in the skin barrier.
Research from the Journal of Investigative Dermatology has shown that babies who develop diverse, balanced skin microbiomes in their first year have stronger barrier function and lower rates of eczema and allergies (source). This is why excessive cleaning or use of antibacterial products can backfire—you're potentially disrupting the beneficial bacteria your baby's skin needs.
When to Seek Professional Help
Most babies navigate barrier development smoothly with basic supportive care. But sometimes, professional intervention is necessary. Contact your pediatrician or a pediatric dermatologist if you notice:
Persistent dryness that doesn't improve with regular moisturizing
Red, inflamed patches that spread or seem to cause discomfort
Cracking, oozing, or bleeding skin
Signs of infection (yellow crusting, increasing redness, warmth, or fever)
Rashes that interfere with sleep or feeding due to discomfort
These could indicate barrier dysfunction that needs more targeted treatment, such as prescription moisturizers, gentle topical steroids, or identification and elimination of specific triggers.
The Long View: Investing in Future Skin Health
Here's something that motivates me and might resonate with you too: the care you provide now has lasting implications. Research increasingly suggests that proper barrier support in infancy may reduce the risk of allergies, asthma, and chronic skin conditions later in life—sometimes called the "atopic march."
The theory goes like this: when the skin barrier is compromised, allergens penetrate more easily, potentially sensitizing the immune system. This early sensitization through the skin may contribute to food allergies, environmental allergies, and respiratory issues down the line. While research is ongoing, several studies have found correlations between infant barrier dysfunction and later development of allergic conditions (source).
By supporting healthy barrier development now—through gentle cleansing, appropriate moisturizing, avoiding unnecessary irritants, and consulting professionals when issues arise—you may be influencing your child's health trajectory in ways that extend far beyond soft baby skin.
The Beauty of Biology
There's something profound about understanding what's happening beneath the surface of your baby's skin. That invisible construction site is a marvel of biology—cells organizing, lipids aligning, beneficial bacteria colonizing, all working toward the goal of a strong, resilient barrier that will protect your child throughout their life.
You don't need to be a dermatologist to support this process. You just need to understand that this delicate skin is doing something extraordinary, and that your choices—what you apply, how often you cleanse, the environment you create—all matter.
So the next time you're gently rubbing in that moisturizer or carefully choosing a product, know that you're not just preventing dry skin. You're actively participating in one of your baby's crucial developmental processes. You're the supportive partner to your baby's skin as it builds its defenses, one microscopic layer at a time.
And honestly? That's one of the most tangible ways you can protect your little one in those early months—supporting the shield they're building for themselves.


News, Voices & Impact
Explore updates, field notes, and stories that showcase our mission and impact.